Understanding Your Arthritis Treatment Plan
You’ve just been diagnosed with an inflammatory form of arthritis – rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), juvenile idiopathic arthritis (JIA) or lupus. You’re in pain, you’re tired and you’re scared. And now you are confused by what your doctor is telling you to do. The treatment plan seems complicated and the drug names unfamiliar.
Don’t let your fear and confusion stop you from taking action. Treating your inflammatory arthritis as soon as you find out you have it is vitally important. Not only do you want to relieve your pain and fatigue as soon as possible, but you want to stop joint and organ damage before it really gets started.
The articles in this section of the website will help you understand your medicine options and help you make decisions with your doctor about your treatment plan. The articles here will give you the basic information you need and will then link you off to more detailed articles in other sections of the site. After you’ve read up on your diagnosis and your treatment options, have a good talk with your doctor about your treatment plan. Talk openly about your expectations, concerns and fears.
Medications for Arthritis Learn about the medicines you can use to treat arthritis and its symptoms.
Whether you have osteoarthritis, rheumatoid arthritis, psoriatic arthritis, or one of the nearly 100 other forms of arthritis and related diseases, you have plenty of medicines available to help. They can ease symptoms, slow the disease down and help you live a full and busy life. Some arthritis-related diseases — such as gout, fibromyalgia and osteoporosis — have medicines just for those diseases and are covered in our Drug Guide.
Here is a breakdown to help you sort out what is best for you.
Analgesics
General pain killers (analgesics) ease mild to moderate pain but don’t do anything for inflammation (hot, swollen joints). Acetaminophen (Tylenol) is available over the counter and is often used for arthritis because it doesn’t hurt your heart and stomach the way nonsteroidal anti-inflammatory agents (NSAIDs) can. But too much can harm your liver so you need to be careful about how much you take. Also watch out for combination products — such as cold, allergy or sleep medicines — that have acetaminophen plus other active ingredients.
Opioids are pain killers that must be prescribed by a doctor. They are very strong and can work well for severe pain. But they do have more side effects than acetaminophen and people can become dependent on them or addicted. Donald Miller, PharmD, Professor, Department of Pharmacy Practice at North Dakota State University in Fargo warns they are not much more useful for long-term use than acetaminophen or NSAIDs.
Medicines that contain both acetaminophen and opioids are also available.
Nonseroidal Anti-inflammatory Drugs (NSAIDs)
NSAIDs relieve pain and inflammation by blocking hormone-like substances called prostaglandins.
Naproxen (Aleve), aspirin and ibuprofen (Motrin, Advil) are available over the counter. Others like indomethacin (Indocin) and celecoxib (Celebrex) require a prescription.
NSAIDS can increase your chances of having a heart attack, stroke or a stomach bleed.
Corticosteroids
Corticosteroids, sometimes called steroids or glucocorticoids, reduce inflammation by acting like your natural hormone cortisol. They work quickly so are good for short-term relief. But they can create problems like weight gain, cataracts and high blood pressure. If you need to take them for a long time, your doctor will have you take only a small amount each day.
Traditional Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs are used to slow or stop the inflammation that causes your joints and disease to get worse. They are an important tool for treating RA, ankylosing spondylitis, psoriatic arthritis, juvenile idiopathic arthritis and lupus. DMARDs weaken your ability to fight germs, so taking them raises your chances for getting infections.
It can take weeks or months for DMARDs to work. One DMARD might not do enough for you, so your doctor may combine two or three at a time. This is called combination therapy.
Methotrexate is the most well known and most used DMARD. It is usually the first drug your doctor will give you after you’ve been diagnosed with RA.
Biologics
Biologics are a special type of DMARD. These powerful drugs work very well for many people with RA and other forms of inflammatory arthritis. They are harder to make than traditional DMARDs, so they can cost more than many of the medicines you may take. Some come as a shot that you give yourself and some have to be given in the doctor’s office through an IV (intravenous infusion). They weaken your ability to fight germs so you may get infections while taking biologics.
One biologic may work very well for some people, but not for others. A biologic may work for you at first, but then stop working after a while. If the first one you try doesn’t work for you, your doctor has other options.
There are five different types of biologics. Each works in a different way to stop what is making you sick.
- Anti-TNFs – also called TNF inhibitors or TNF blockers
- Interleukin-6 (IL-6) inhibitors
- Interleukin-1 (IL-1) receptor antagonists B-cell inhibitors
- Co-stimulation modulators
Targeted DMARDs
Unlike traditional DMARDs that slow your disease by holding down your body’s whole immune system, a couple of targeted DMARDs have come out that are more specific. These medicines are taken by mouth.
- Janus kinases (JAK) inhibitors: Your doctor may have you take this medicine if methotrexate doesn’t work for you.
- Phosphodiesterase 4 (PDE 4) inhibitors: Unlike other DMARDs, this medicine doesn’t increase your chance of getting a serious infection.
Benefits and Risks of Arthritis Medicines All medicines have risks and benefits to weigh before you take them.
There is no cure for rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS) or other inflammatory diseases, but there are treatments. An ever-increasing collection of drugs, used alone or together, have made low disease activity or remission possible.
The goal is to treat these diseases aggressively right after diagnosis to prevent joint and organ damage before it starts. Along with medicines that slow or stop the disease, you may take medicines to ease your pain and other symptoms. You and your doctor will have to weigh the risks and benefits of each drug before you decide to take it. Here’s a snapshot of the medicines your doctor will most likely prescribe for you or that you’ll buy over the counter.
Acetominophen
Benefits: Acetaminophen relieves mild-to-moderate pain and reduces fever. It is cheap, easy on the stomach and does not increase your chances of having heart problems (as some other painkillers can).
Risks: This medicine is found in hundreds of prescription and over-the-counter (OTC) drugs, making it easy to take too much by mistake. Too much acetaminophen can damage your liver. Drinking more than two alcoholic drinks a day for men and more than one glass per day for women can add to the chance of harming your liver. Acetaminophen does not treat inflammation.
Opioids
Benefits: These prescription-only medicines are strong painkillers. Some are also used to soothe a bad cough or stop severe diarrhea.
Risks: Taking opioid medicines can make you dizzy, sleepy and constipated. If you take them for more than a short time, you may need to take more to get the same pain relief (this is called tolerance). If you stop taking them all at once, you may go into withdrawal and feel sick (this is called physical dependence). Some people can become addicted to opioids, but this is not the same as tolerance or dependence.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Benefits: NSAIDs relieve pain, reduce fever and fight inflammation. They are available in over-the-counter and prescription strengths. Aspirin is an NSAID that can reduce your chance of having a heart attack or stroke if you have cardiovascular disease.
Risks: NSAIDs other than aspirin can increase your chances of having a heart attack or stroke. All NSAIDs can be hard on the stomach and can sometimes result in a stomach bleed.
“We shy away from these if someone has a history of heart disease or chronic gastrointestinal issues; but if someone has mild stomach symptoms with use, we can prescribe these drugs with a proton pump inhibitor to protect the stomach,” says Melissa Bussey, MD, an assistant professor in the Division of Allergy/Immunology/Rheumatology of Loyola University Chicago Stritch School of Medicine.
Corticosteroids
Benefits: Corticosteroids work in the same way as your natural hormone cortisol to reduce inflammation. Steroids give quick pain and inflammation relief, such as during a flare. They also slow down your immune system, which can help control autoimmune diseases.
Risks: The side effects of steroids depend on how you take them, how long you take them, and how much you take. Some possible side effects include glaucoma (increased pressure in the eye), cataracts (clouding of the lens of the eye), fluid retention, mood and behavior changes, higher blood fat and blood sugar levels, increased appetite, and thinning bones and skin.
Traditional DMARDs
Benefits: Traditional disease-modifying antirheumatic drugs (DMARDs) suppress your immune system and are used to fight inflammatory forms of arthritis. They ease symptoms, slow the disease down and slow joint damage. They can be taken in pill form, but some are also available in a shot that you give to yourself.
Risks: Because DMARDs hold back your immune system from overacting, they make it harder for you to fight infections. They also may slightly increase your chance of having certain cancers. Other side effects that could happen depend on which drug you take, but could include liver problems, low blood cell counts, diarrhea, headache, hair loss, lack of energy, rash or itching, upset stomach and weight loss. They can take several weeks to work, so your doctor may also prescribe an NSAID or corticosteroid along with a DMARD so you’ll feel better right away.
Biologic DMARDs
Benefits: Drugs in this subset of DMARDs work on specific parts of the immune system and do a good job of stopping inflammation and slowing the disease down.
Risks: Biologics are not available as pills; they come as shots or intravenous (IV) infusions. Biologics weaken your ability to fight germs so you may get infections while taking biologics and "silent" infections (like tuberculosis and hepatitis B) may come back. Some biologic drugs may increase your chance of getting certain types of cancer, cause heart failure or cause multiple sclerosis. Side effects that some people get include headache, injection site reaction (itching, redness, swelling) and infusion reaction (difficulty breathing, rapid or weak pulse, rash, nausea, vomiting).
Targeted DMARDs
Benefits: Targeted DMARDs work in very specific ways instead of suppressing the body's entire immune system. This means you may have fewer side effects than when you take traditional DMARDS. These medicines come in pill form, which is good for people who don’t like needles or can’t get to the doctor’s office for an IV (intravenous infusion).
Risks: Side effects of targeted DMARDs include mood changes, diarrhea and upset stomach. Any medicine that holds down your immune system can decrease your ability to fight germs. One of the targeted DMARDs, apremilast, does not appear to increase your chance of getting a serious infection.
Managing Arthritis is More Than Treating PainThe goal of treatment is to prevent long-term joint and organ damage.
All you can think about is being able to walk, bend and reach without joint pain. While that directly impacts your daily life, managing your arthritis is about more than just pain relief.
“Pain relief certainly shows that you are on the right track,” says Eric Matteson, MD, professor of medicine and rheumatologist at Mayo Clinic in Rochester, Minnesota. “There is often more that can be done to cool underlying, systemic inflammation and help prevent long-term damage to the joints and other organs that can occur with rheumatoid arthritis (RA), psoriatic arthritis (PsA) and ankylosing spondylitis (AS).”
A complete arthritis treatment plan eases pain and inflammation, slows joint and organ damage, and improves physical function and quality of life.
Reach for Remission
Rather than just soothing pain and allowing you to “get by,” doctors have the tools and medicines available to completely quiet many types of inflammatory arthritis. When your symptoms are nearly gone and the doctor says your joints aren’t inflamed anymore, that’s called remission.
If you start treating the disease as soon as you find out you have it, and if you keep taking the medicines your doctor prescribes, you can go into remission. When treated early with DMARDs and biologics, remission rates can be as high as 60% — and sometimes even higher. Even if you don’t get all the way down to zero symptoms, you will have less pain, be able to move better, have a good quality of life, and your chances of developing other problems like heart disease will be less.
Treat-to-Target
Some doctors use a strategy called treat-to-target when working with you to come up with a treatment plan. The idea is that you and your doctor work closely together to decide on a goal (the ideal goal is low disease activity or remission) and a plan to reach that goal. You then have regular checkups to see how you’re doing (every 3 months, for example). Your doctor will adjust your medicines and other treatments until you reach your goal.
There are many ways to measure your disease activity during those checkups. David Pisetsky, MD, PhD, a professor of medicine and immunology and chief of rheumatology at Duke University Medical Center in Durham, North Carolina, says, “We can get inflammation down so people feel no pain, but this doesn’t tell the full story. When inflammation levels are high, it’s easy to see damage on X-rays, but when levels are low, it is more difficult to know what is going on.”
Blood tests like erythrocyte sedimentation rate (ESR or “sed rate”) and C-reactive protein (CRP) measure body-wide inflammation. However, they are not sensitive enough to pick up lower activity that may still be harming your joints and organs. Newer tests (such as Vectra DA) look at many markers to come up with a total disease score. Dr. Pisetsky says doctors are looking at those to see which can best measure low disease activity.
Treat to target for RA is becoming common, and doctors are also starting to use treat to target in PsA.
Lifestyle Changes Matter Too
Medicines don’t work on their own. Any medicine will work better if you combine it with lifestyle changes. Losing weight (when needed), keeping your cholesterol and blood pressure under control, and stopping smoking will all improve your health and quality of life.
Physical and occupational therapy, exercise, disease education, and complementary therapies can all be part of your total arthritis wellness plan. Dr. Matteson says, “Combining all, or most, of these elements in your personalized arthritis treatment plan and checking in with your rheumatologist regularly to monitor progress remain the best ways to take back your health and stay pain-free.”
Sticking to Your Medicine Plan Matters
Even if you start to feel better or don’t like medication side effects, and you want to stop taking a medication, don’t. Low-level inflammation throughout your body may still be causing joint and organ damage. It’s important to stick with your treatment plan and talk to your doctor about your concerns. If you don’t take your medicine, your doctor won’t know what is or is not working so she won’t know when or how to switch your medications.
Don’t Settle for “Good Enough”
“What happens is that people achieve a level of tolerable pain, meaning that they can deal with it and live their lives,” says Dr. Pisetsky. “Yes, they could do better, but they are getting along OK and are grateful for that.”
Until you reach low disease activity or remission, don’t give up. You don’t need to settle for just getting by – and you shouldn’t let your doctor either. Just because you feel “okay” doesn’t mean your disease is under control. Keep working with your doctor to find a treatment that eliminates your inflammation and pain.
Role of Advanced Therapies in ArthritisRheumatologists are treating inflammatory arthritis with targeted DMARDs and biologics.
New super-specific medicines and new uses of existing drugs are changing the way rheumatoid arthritis (RA), psoriatic arthritis (PsA) and other inflammatory diseases are treated. In the not-too-distant past, arthritis often meant joint deformity and disability, and even early death.
Not anymore.
Earlier diagnosis and advanced medicines have changed the landscape of arthritis treatment. As a result, people with arthritis are now living longer and healthier lives than ever before.
“In the 1980s and 1990s, the goal was to control disease activity as much as we could, but now our goal is to treat these diseases aggressively early on to prevent progression, downstream consequences including heart risks and the need for surgery,” says Linda A. Russell, MD, an assistant attending physician at the Hospital for Special Surgery in New York City.
Doctors call this strategy “treat to target” and it’s helping people who have inflammatory diseases live better.
There is no cure for RA, PsA or ankylosing spondylitis (AS). But by pairing the right medicines with the right person and not being afraid to make changes, remission – no signs of active disease — is possible for many.
Starting with Traditional DMARDs
Traditional disease modifying anti-rheumatic drugs (DMARDs) are usually the first medicines used for inflammatory diseases like RA, Dr. Russell says.
As their name suggests, these drugs slow the disease down. They may be used together, with other types of DMARDs, with nonsteroidal anti-inflammatory drugs (NSAIDs) or with corticosteroids. Using two or three traditional DMARDs together (called combination therapy) was once common in RA treatment. Research shows these combinations can still hold their own against some of the newer drugs.
“The traditional DMARDs are so much cheaper than some of the newer medications, and have been around so much longer, that we try a DMARD first. But we don’t wait too long to move on,” Dr. Russell says. If, after a three-month trial, symptoms aren’t improving, another DMARD or a biologic may be added to the mix, she says.
Moving to Advanced Therapies
Biologics work on specific parts of the immune system, making them more precise than traditional DMARDs. These powerful medicines are given as a shot or in a doctor’s office through an IV (intravenous infusion). “Most often, patients take these drugs with methotrexate, as the mix of medicines is more helpful than either alone,” says Dr. Russell.
Usually the first biologic your doctor will prescribe is one that blocks tumor necrosis factor-α (TNF-α). If the first anti-TNF drug you try doesn’t work or does work at first but stops working, you may try another anti-TNF. If you have a serious side effect or you don’t get relief from the second anti-TNF, there are several other biologics your doctor can prescribe.
The newest kids on the block are called “targeted DMARDs” and these are usually tried when biologics fail, says David Pisetsky, MD, PhD, a professor of medicine and immunology and chief of rheumatology at Duke University Medical Center in Durham, North Carolina.
Unlike the traditional DMARDs, targeted DMARDs are super-specific. They target different players in the inflammation process than biologics. Unlike biologics, they come in pill form.
“Biologics have been around longer than targeted DMARDs so they are typically used first, but in the future, targeted DMARDs may be started sooner,” Dr. Pisetsky says.
Cost, preferences about oral versus injectable medicines, and medical history all factor into the decision about which drugs to try and when to try them. “Different patients respond to different drugs,” says Melissa Bussey, MD, an assistant professor in the division of allergy, immunology and rheumatology of Loyola University Chicago Stritch School of Medicine. “The good news here is that we have many options to try.”
Different Ways to Take Arthritis MedicationsYour doctor can prescribe a variety of medicines to treat your arthritis and its symptoms. Here’s a look at drug delivery methods for different arthritis medications.
Oral Medicines
Many of the drugs you take for arthritis – including acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), some disease-modifying antirheumatic drugs (DMARDs) and corticosteroids – come in pill form. Instructions vary, but typically you’ll swallow the pill(s) with a big sip of water.
The label might also specify that you take your medicine on a full stomach, but it may matter what you eat or drink. Once your body digests the pill, its contents will be absorbed into your bloodstream and take effect.
Talk to your doctor before trying to cut, crush or chew your pills. While some DMARDs may be taken as a divided dose, there are others that must be swallowed whole. If you have trouble swallowing pills, some medications are available as liquids.
Topical Medicines
Topicals deliver medicines through your skin. NSAIDs, salicylates and capsaicin are available as creams or gels that you rub on your skin. Opioid medicines, NSAIDs and lidocaine are available in as a patch you apply to the skin. A patch delivers a steady dose of medicine into your bloodstream over several hours. You will leave it on for 12 or more hours, depending on the drug, and then remove it. If you have psoriatic arthritis or another skin condition, talk to your doctor before using a topical medicine.
Self-Injections
Some people take the DMARD methotrexate as an injection because it may be more effective that way. Several biologic drugs (a subset of DMARDs) have to be injected because there are no pill forms available. While it can be scary to think about using a needle on yourself, your doctor or nurse will show you how to prepare and inject the drug. You should get the hang of it fairly quickly. If you’d prefer not to do it yourself, ask a friend or family member to learn how and give you the injections.
Injectables come two ways depending on the drug: with an auto-injector pen or a syringe. Some injectables need refrigeration. If you travel often for work or pleasure, you’ll need to plan ahead to have access to a fridge.
The needle is shorter than the ones you’re used to getting at your doctor’s office. You’ll place the needle into an area of fat between the skin and muscle, called the subcutaneous layer. The best places to give yourself an injection are in the side of your thigh or the bottom part of your stomach (a few inches away from your bellybutton). If someone is helping you, they can give you the injection in the back of your arm. Don’t use the same spot each time you inject to prevent soreness. You can rub an ice cube on your skin first to numb the region. Then, clean the area with an alcohol swab.
With the auto-injector, the medicine is already inside the pen. You simply take off the cap and hold the device firmly against your skin. Then you press and hold the button on the pen, and the needle injects the medicine into your subcutaneous layer.
Syringes may be either prefilled or empty. You’ll have to fill the empty ones yourself from a multi-use vial. You pinch your skin with a bit of fat, quickly insert the needle, and push down the plunger to inject the medicine.
Once you’re done injecting with either an auto-injector or syringe, dispose of the needle in a special container you get from the pharmacy. After the injection, some people develop a skin reaction at the site of the needle puncture. Injection-site reactions cause symptoms like redness, itching, pain and possibly a rash. If you see these symptoms, call your doctor.
Infusions
Several of the biologic drugs need to go straight into your bloodstream to be effective. You’ll get these drugs as an infusion, which is through a needle placed into a vein (called an IV). You’ll visit the doctor’s office, a hospital or an infusion center to get the drug. Infusions are given on different schedules, ranging from weeks to months apart. You may need to take time off work and plan around your travel schedule to get your infusions.
About 30 minutes before your infusion, you may get a corticosteroid medicine through a vein to prevent you from having a reaction to the infusion drug. While you get the infusion, the nurses will check your breathing rate and blood pressure and monitor for signs of a reaction to the biologic. If you do have a reaction, your doctor will give you an antihistamine, acetaminophen, or a steroid drug to treat it.
Wear loose-fitting clothing during your infusion to make it easier for the medical team to monitor your vital signs, and to keep you more comfortable while you wait. Bring a book or music player. Some infusions can take two hours or longer. You will need to watch for signs of an infusion or injection-site reaction at home, because some reactions can occur up to 14 days after treatment. Signs of an infusion reaction include flushing, rash, fever, headache, shortness of breath, chest pain and heart palpitations. Call your doctor if you have signs of an infusion reaction.
Sticking With Your Arthritis Treatment PlanTaking your medicines like you’re supposed to can be tough. But it’s important.
Treating rheumatoid arthritis (RA), psoriatic arthritis (PsA) and other inflammatory forms of arthritis can be hard with all those pills, shots and trips to the doctor. Add worries about side effects and costs, and it’s easy to see why some people don’t start or stick to their medicine schedule.
Common Problem
Doctors find that for people with inflammatory arthritis, taking their medicine is a problem with both traditional disease-modifying antirheumatic drugs (DMARDs) and biologics. Studies find that between 35% and 85% of people with RA don’t always take their medicines as prescribed.
“With biologics one assumption has been that if you prescribe this powerful drug that’s very expensive and effective, that will make people more adherent [than with traditional DMARDs]. But this hasn’t been borne out by research,” says Ian Bruce, MD, professor of rheumatology at the University of Manchester in the UK. He published a study in 2015 in Rheumatology that looked at how well 329 people with RA stuck to their schedule of adalimumab (Humira) shots. About two-thirds did not take their shots when and how often they were supposed to.
Not taking medicines or taking them wrong can lead to disease flares and joint damage, says Maria Suarez-Almazor, MD, PhD, chief of the section of rheumatology at MD Anderson Cancer Center in Houston. “[Inflammatory forms of arthritis like] RA progress slowly, so it can be difficult for patients to realize they are damaging themselves when they stop medications,” she says.
It can also cloud the picture for doctors, says Dr. Bruce. “When people aren’t doing as well as we think they should be, we assume it’s because the drug isn’t working; oftentimes it’s because the drug isn’t being taken properly.”
What’s Going On
Reasons people give for not filling or taking medicine are mixed. The cost can be one issue, says Elizabeth Salt, PhD, assistant professor of medicine in the division of rheumatology at the University of Kentucky College of Medicine in Lexington. “Many people have large copayments, hundreds of dollars a month, and though doctor’s offices work with drug companies to get assistance, it can be a big burden.”
Other reasons people give for not taking medicine is that they don’t think the medicine is needed or they are afraid of having a bad reaction to it.
Dr. Bruce says that when people understand inflammatory arthritis is a lifelong disease that needs lifelong treatment, they are more likely to take their medicine. And if they believe the drugs will control the disease, they will take their medicine. However, some patients feel that a drug is of little value because it hasn’t made them completely symptom-free. “Sometimes we can’t get 100% pain relief, but that doesn’t mean the drug isn’t helping control symptoms and preventing joint damage,” says Dr. Suarez-Almazor.
On the flip side are people who feel so much better they don’t see a reason to keep taking the medicines. “Patients may be able to wean off medications or take lower doses, but that is a conversation they need to have with their physician. About half of people flare when they stop biologics,” says Dr. Suarez-Almazor.
Doctors will usually talk with you about side effects of arthritis medicines, but sometimes they don’t ease your fears or address your real concerns.
“People can be concerned about cancer with biologics, though large databases show they don’t increase cancer risk,” says Dr. Bruce. “Patients also worry about fertility or about effects on their appearance – hair loss and weight gain, for example – but they may not bring this up with the doctor.”
Talk To Your Doctor
Many problems you have about taking your medicine can be made better by talking about them. Nurses in your doctor’s office can explain your disease and the medicines you’ve been asked to take. They may be able to help you get discounts on your costly drugs, and they can help find ways to remind you take your medicines.
Working with your doctor to make decisions about your treatment will put you more in control. Talk about your worries with your doctor and be sure to go over the pros and cons of the medicines. Then together you can decide what’s best for you. Being part of the decision will help you stick with the decisions you made.
Dr. Suarez-Almazor agrees. “If you’re concerned a drug may not be useful or you’ve heard about a bad outcome in a friend or relative or on the Internet, bring it up with your physician,” she says. “Everything has a price … there’s always risk with the medications you take. But you might have more risks from not taking the medication, because your disease can also hurt you.”
Above all, be open about your fears. “Nowadays we have many treatment options,” she says. “If patients don’t like the medication because they feel they are having adverse effects or they don’t have the quality of life they want, there are other medications.”
DMARDs Drug Guide
Disease-modifying anti-rheumatic drugs (DMARDs) work to slow or stop the inflammatory process that can damage joints and internal organs.
There are three subsets of DMARDs. So-called “traditional” DMARDs are, for the most part, taken orally and have a broad immune suppressant effect. Biologics, taken by self-injection or infusion, introduced in the late 1990s, target specific immune system molecules. The newest DMARDs, here labeled “targeted,” are oral drugs that also target specific immune system molecules.
Because DMARDs interact with the immune system, they can decrease the ability to fight infections and may increase the risk of certain cancers. Some DMARDs are prescribed together as “combination therapy” – to be used with other DMARDs or a biologic.
Your doctor may also prescribe an NSAID and/or corticosteroid along with a DMARD, for use until the DMARD takes effect.
Download your free copy of our DMARDs Guide for information on the disease-modifying antirheumatic drugs used to treat arthritis, including brand names such as Rasuvo (methotrexate), Xeljanz (tofacitinib) and Azasan (azathioprine).
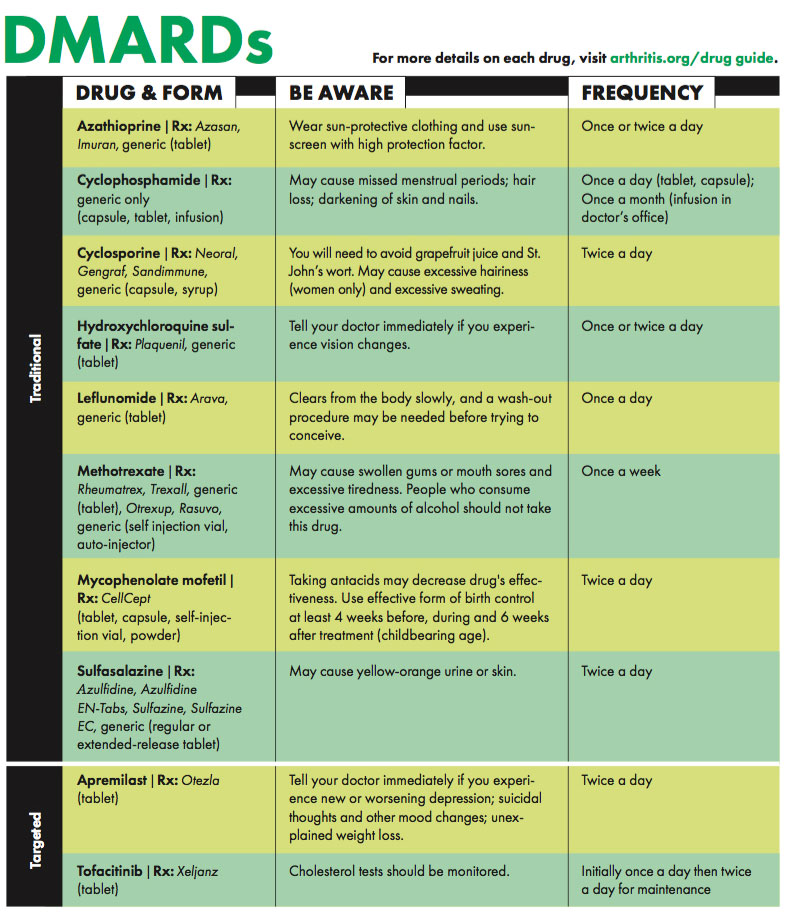
Download Your DMARDs Guide
To download your own copy of our DMARDs Drug Guide and get details about all 10 disease-modifying antirheumatic drugs, including brand names and modes of administration.
Our DMARDs drug guide also includes:
- What you should learn before starting DMARDs
- Side effects
- Drug interactions
- Symptoms to be aware of
- Pregnancy warnings
- Details on DMARDs
Biologics Drug Guide
Biologic response modifiers, or biologics, target proteins, cells and pathways responsible for triggering the symptoms and damage from autoimmune and inflammatory types of arthritis. The drugs work by interfering with one of the following: tumor necrosis factor (TNF), B cells (a type of white blood cell), T cells (another type of white blood cell) and interleukins (including IL-1, IL-6, IL-12 and IL-23).
Biologics increase the risk of serious infections and may cause "silent" infections (e.g., tuberculosis and hepatitis B) to reoccur. Some may increase the risk of certain types of cancer, cause new or worsening congestive heart failure or multiple sclerosis.
Many biologics are not recommended during pregnancy and nursing. You should tell your doctor if you are pregnant, nursing or plan to become pregnant.
Download your free copy of our Biologics Guide for information on the biologics drugs used to treat arthritis, including brand names such as Humira, Acemtra (and Actemra methotrexate) and Xeljanz (tofacitinib).
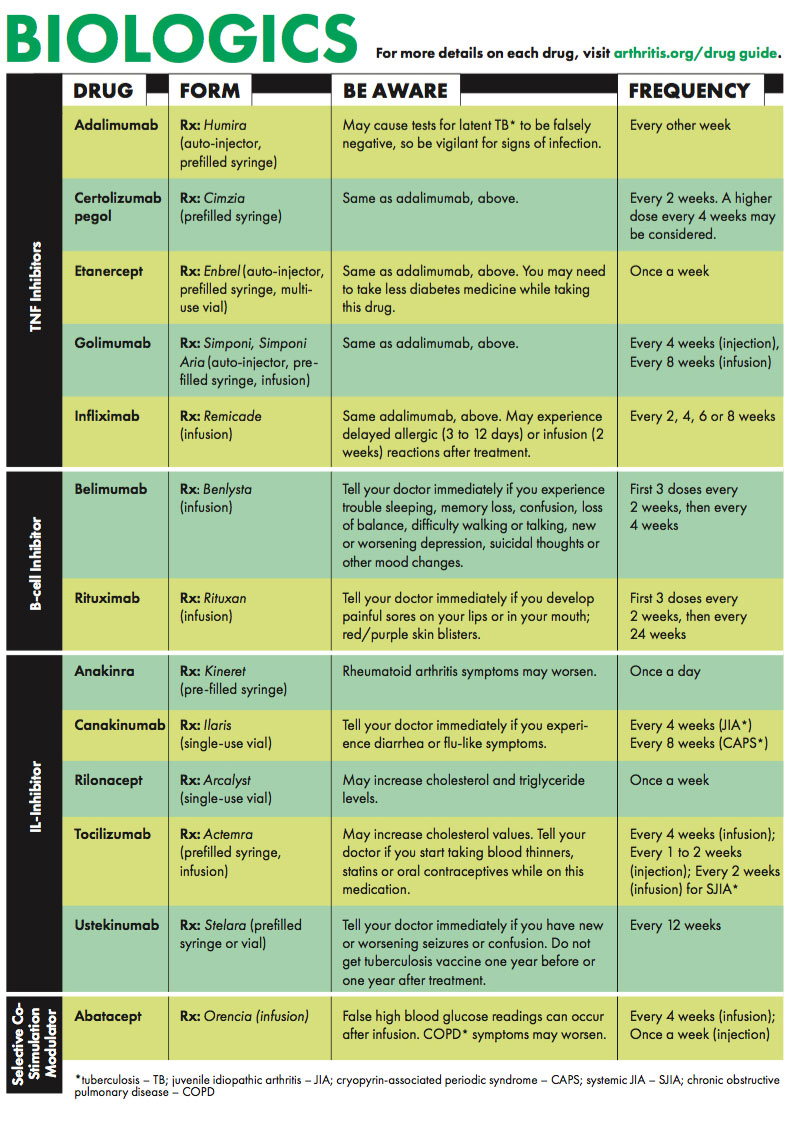
Our biologics drug guide includes:
- What you should learn before starting biologics
- Side effects
- Drug interactions
- Symptoms to be aware of
- Pregnancy warnings
- Details on biologics


